In some animals, including vertebrates, echinoderms, insects (mid-gut) and molluscs, the stomach is a muscular, hollow, dilated part of the alimentary canal which functions as an important organ of the digestive tract. It is involved in the second phase of digestion, following mastication (chewing). The stomach is located between the oesophagus and the small intestine. It secretes protein-digesting enzymes and strong acids to aid in food digestion, (sent to it via oesophageal peristalsis) through smooth muscular contortions (called segmentation) before sending partially digested food (chyme) to the small intestines.
The word stomach is derived from the Latin stomachus which is derived from the Greek word stomachos, ultimately from stoma (στόμα), "mouth". The words gastro- and gastric (meaning related to the stomach) are both derived from the Greek word gaster (γαστήρ).
Two sphincters keep the contents of the stomach contained. They are the esophageal sphincter (found in the cardiac region, not an anatomical sphincter) dividing the tract above, and the Pyloric sphincter dividing the stomach from the small intestine.
The stomach is surrounded by parasympathetic (stimulant) and orthosympathetic (inhibitor) plexuses (networks of blood vessels and nerves in the anterior gastric, posterior, superior and inferior, celiac and myenteric), which regulate both the secretions activity and the motor (motion) activity of its muscles.
In adult humans, the stomach has a relaxed, near empty volume of about 45 ml. Because it is a distensible organ, it normally expands to hold about 1 litre of food,[4] but can hold as much as 2-3 litres. The stomach of a newborn human baby will only be able to retain about 30ml.

Like the other parts of the gastrointestinal tract, the stomach walls are made of the following layers, from inside to outside:

Different types of cells are found at the different layers of these glands:
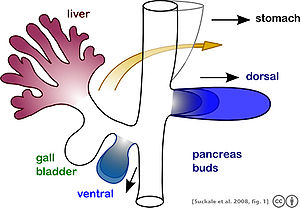
Other than gastrin, these hormones all act to turn off the stomach action. This is in response to food products in the liver and gall bladder, which have not yet been absorbed. The stomach needs only to push food into the small intestine when the intestine is not busy. While the intestine is full and still digesting food, the stomach acts as storage for food.
The gastric lining is usually divided into two regions, an anterior portion lined by fundic glands, and a posterior with pyloric glands. Cardiac glands are unique to mammals, and even then are absent in a number of species. The distributions of these glands vary between species, and do not always correspond with the same regions as in man. Furthermore, in many non-human mammals, a portion of the stomach anterior to the cardiac glands is lined with epithelium essentially identical to that of the oesophagus. Ruminants, in particular, have a complex stomach, the first three chambers of which are all lined with oesophageal mucosa.[13]
In birds and crocodilians, the stomach is divided into two regions. Anteriorly is a narrow tubular region, the proventriculus, lined by fundic glands, and connecting the true stomach to the crop. Beyond lies the powerful muscular gizzard, lined by pyloric glands, and, in some species, containing stones that the animal swallows to help grind up food.[13]

The word stomach is derived from the Latin stomachus which is derived from the Greek word stomachos, ultimately from stoma (στόμα), "mouth". The words gastro- and gastric (meaning related to the stomach) are both derived from the Greek word gaster (γαστήρ).
Contents[hide] |
[edit] Role in digestion
Bolus (masticated food) enters the stomach through the oesophagus via the oesophageal sphincter. The stomach releases proteases (protein-digesting enzymes such as pepsin) and hydrochloric acid, which kills or inhibits bacteria and provides the acidic pH of 2 for the proteases to work. Food is churned by the stomach through muscular contractions of the wall - reducing the volume of the fundus, before looping around the fundus[3] and the body of stomach as the boluses are converted into chyme (partially digested food). Chyme slowly passes through the pyloric sphincter and into the duodenum, where the extraction of nutrients begins. Depending on the quantity and contents of the meal, the stomach will digest the food into chyme anywhere between 40 minutes and a few hours.[edit] Anatomy of the stomach
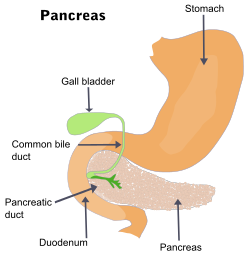
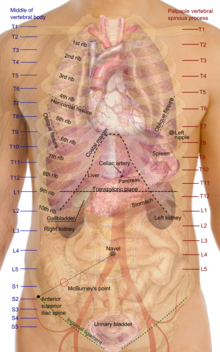
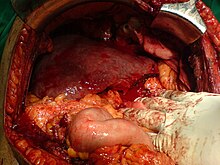
The stomach lies between the oesophagus and the duodenum (the first part of the small intestine). It is on the left upper part of the abdominal cavity. The top of the stomach lies against the diaphragm. Lying behind the stomach is the pancreas. The greater omentum hangs down from the greater curvature.Two sphincters keep the contents of the stomach contained. They are the esophageal sphincter (found in the cardiac region, not an anatomical sphincter) dividing the tract above, and the Pyloric sphincter dividing the stomach from the small intestine.
The stomach is surrounded by parasympathetic (stimulant) and orthosympathetic (inhibitor) plexuses (networks of blood vessels and nerves in the anterior gastric, posterior, superior and inferior, celiac and myenteric), which regulate both the secretions activity and the motor (motion) activity of its muscles.
In adult humans, the stomach has a relaxed, near empty volume of about 45 ml. Because it is a distensible organ, it normally expands to hold about 1 litre of food,[4] but can hold as much as 2-3 litres. The stomach of a newborn human baby will only be able to retain about 30ml.
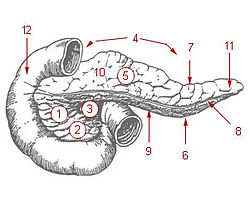
[edit] Sections
The stomach is divided into 4 sections, each of which has different cells and functions. The sections are:| Cardia | Where the contents of the oesophagus empty into the stomach. |
| Fundus | Formed by the upper curvature of the organ. |
| Body or Corpus | The main, central region. |
| Pylorus | The lower section of the organ that facilitates emptying the contents into the small intestine. |
[edit] Blood supply

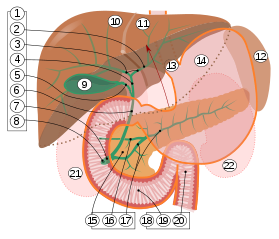
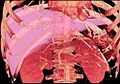
Schematic image of the blood supply to the stomach: left and right gastric artery, left and right gastro-omental artery and short gastric artery.[5]
The lesser curvature of the stomach is supplied by the right gastric artery inferiorly, and the left gastric artery superiorly, which also supplies the cardiac region. The greater curvature is supplied by the right gastroepiploic artery inferiorly and the left gastroepiploic artery superiorly. The fundus of the stomach, and also the upper portion of the greater curvature, are supplied by the short gastric artery.
Like the other parts of the gastrointestinal tract, the stomach walls are made of the following layers, from inside to outside:
| mucosa | The first main layer. This consists of the epithelium and the lamina propria (composed of loose connective tissue), with a thin layer of smooth muscle called the muscularis mucosae separating it from the submucosa beneath. |
| submucosa | This layer lies over the mucosa and consists of fibrous connective tissue, separating the mucosa from the next layer. The Meissner's plexus is in this layer. |
| muscularis externa | Over the submucosa, the muscularis externa in the stomach differs from that of other GI organs in that it has three layers of smooth muscle instead of two.
|
| serosa | This layer is over the muscularis externa, consisting of layers of connective tissue continuous with the peritoneum. |

Micrograph showing a cross section of the stomach wall, in the body portion of the stomach. H&E stain.
[edit] Glands
The epithelium of the stomach forms deep pits. The glands at these locations are named for the corresponding part of the stomach:| Cardiac glands (at cardia) | Pyloric glands (at pylorus) | Fundic glands (at fundus) |
 |  |  |
| Layer of stomach | Name | Secretion | Region of stomach | Staining |
| Isthmus of gland | Mucous neck cells | mucus gel layer | Fundic, cardiac, pyloric | Clear |
| Body of gland | parietal (oxyntic) cells | gastric acid and intrinsic factor | Fundic only | Acidophilic |
| Base of gland | chief (zymogenic) cells | pepsinogen | Fundic only | Basophilic |
| Base of gland | enteroendocrine (APUD) cells | hormones gastrin, histamine, endorphins, serotonin, cholecystokinin and somatostatin | Fundic, cardiac, pyloric | - |
[edit] Control of secretion and motility
The movement and the flow of chemicals into the stomach are controlled by both the autonomic nervous system and by the various digestive system hormones:| Gastrin | The hormone gastrin causes an increase in the secretion of HCl from the parietal cells, and pepsinogen from chief cells in the stomach. It also causes increased motility in the stomach. Gastrin is released by G-cells in the stomach in response to distenstion of the antrum, and digestive products(especially large quantities of incompletely digested proteins). It is inhibited by a pH normally less than 4 (high acid), as well as the hormone somatostatin. |
| Cholecystokinin | Cholecystokinin (CCK) has most effect on the gall bladder, causing gall bladder contractions, but it also decreases gastric emptying and increases release of pancreatic juice which is alkaline and neutralizes the chyme. |
| Secretin | In a different and rare manner, secretin, produced in the small intestine, has most effects on the pancreas, but will also diminish acid secretion in the stomach. |
| Gastric inhibitory peptide | Gastric inhibitory peptide (GIP) decreases both gastric acid release and motility. |
| Enteroglucagon | enteroglucagon decreases both gastric acid and motility. |
[edit] EGF in gastric defense
Epidermal growth factor or EGF results in cellular proliferation, differentiation, and survival.[6] EGF is a low-molecular-weight polypeptide first purified from the mouse submandibular gland, but since then found in many human tissues including submandibular gland, parotid gland. Salivary EGF, which seems also regulated by dietary inorganic iodine, plays also an important physiological role in the maintenance of oro-oesophageal and gastric tissue integrity. The biological effects of salivary EGF include healing of oral and gastroesophageal ulcers, inhibition of gastric acid secretion, stimulation of DNA synthesis as well as mucosal protection from intraluminal injurious factors such as gastric acid, bile acids, pepsin, and trypsin and to physical, chemical and bacterial agents.[7][edit] Stomach as nutrition sensor
The stomach can "taste" sodium glutamate using glutamate receptors[8] and this information is passed to the lateral hypothalamus and limbic system in the brain as a palatability signal through the vagus nerve.[9] The stomach can also sense independently to tongue and oral taste receptors glucose,[10] carbohydrates[11] proteins,[11] and fats.[12] This allows the brain to link nutritional value of foods to their tastes.[10][edit] Diseases of the stomach
Main article: Stomach disease
Historically, it was widely believed that the highly acidic environment of the stomach would keep the stomach immune from infection. However, a large number of studies have indicated that most cases of peptic ulcers, gastritis, and stomach cancer are caused by Helicobacter pylori infection.[edit] In other animals
Although the precise shape and size of the stomach varies widely among different vertebrates, the relative positions of the oesophageal and duodenal openings remain relatively constant. As a result, the organ always curves somewhat to the left before curving back to meet the pyloric sphincter. However, lampreys, hagfishes, chimaeras, lungfishes, and some teleost fish have no stomach at all, with the oesophagus opening directly into the intestine. These animals all consume diets that either require little storage of food, or no pre-digestion with gastric juices, or both.[13]
The gastric lining is usually divided into two regions, an anterior portion lined by fundic glands, and a posterior with pyloric glands. Cardiac glands are unique to mammals, and even then are absent in a number of species. The distributions of these glands vary between species, and do not always correspond with the same regions as in man. Furthermore, in many non-human mammals, a portion of the stomach anterior to the cardiac glands is lined with epithelium essentially identical to that of the oesophagus. Ruminants, in particular, have a complex stomach, the first three chambers of which are all lined with oesophageal mucosa.[13]
In birds and crocodilians, the stomach is divided into two regions. Anteriorly is a narrow tubular region, the proventriculus, lined by fundic glands, and connecting the true stomach to the crop. Beyond lies the powerful muscular gizzard, lined by pyloric glands, and, in some species, containing stones that the animal swallows to help grind up food.[13]

Comparison of stomach glandular regions from several mammalian species. Yellow: oesophagus; green: aglandular epithelium; purple: cardiac glands; red: gastric glands; blue: pyloric glands; dark blue: duodenum. Frequency of glands may vary more smoothly between regions than is diagrammed here. Asterisk (ruminant) represents the omasum, which is absent in Tylopoda (Tylopoda also has some cardiac glands opening onto ventral reticulum and rumen[14]) Many other variations exist among the mammals.[15][16]
[edit] See also
- Bariatric Surgery, Weight Loss Surgery
- Foveolar cells, mucous producing cells of the stomach
- Peristalsis, muscular movement that occurs in the stomach
- Borborygmus, growling of stomach
- Digestion
- Gastroesophageal reflux disease
- Discovery and Development of Proton Pump Inhibitors